We Welcome Referrals.
Physicians and other healthcare providers are encouraged to refer patients to our pain clinic for primary care, secondary care as well as for post surgery rehabilitation.
If you require further information specific to Richard A Connell, DOM, LAC, his acupuncture clinic in Galena, Illinois or about the therapies we provide, you are welcome to click here to check out our front page or call us at 815 238 3803 to speak with our office directly.
Physicians and other healthcare providers are encouraged to refer patients to our pain clinic for primary care, secondary care as well as for post surgery rehabilitation.
If you require further information specific to Richard A Connell, DOM, LAC, his acupuncture clinic in Galena, Illinois or about the therapies we provide, you are welcome to click here to check out our front page or call us at 815 238 3803 to speak with our office directly.
Acupuncture For Pain: Seven Questions Answered
A Physician Directed Review of Research
This article will help make sense of this growing body of knowledge by summarizing the latest evidence and addressing seven common questions about acupuncture for pain conditions. Applying this information will give you the confidence to counsel patients appropriately and decide if acupuncture fits within their pain management plan.
J Fam Pract. 2018 April;67(4):224-226,228-230
Author(s): Russell Lemmon, DO
Author and Disclosure Information: Is acupuncture an effective treatment for pain? Are there any adverse effects? Learn the answers to these and other questions in this review.
PRACTICE RECOMMENDATIONS
Recommend acupuncture as a prophylactic treatment for migraine headaches. A
Recommend acupuncture as a treatment option for chronic low back pain. A
Consider using acupuncture as an adjunctive treatment in the management of fibromyalgia symptoms. B
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
An estimated 39.4 million US adults suffer from persistent pain,(1) and the National Institutes of Health indicate that pain affects more Americans than diabetes, heart disease, and cancer combined.(2)
As physicians, we know that conventional options to manage chronic pain leave much to be desired and that more evidence-based treatment options are sorely needed. Patients know this, too, and turn to complementary therapies for pain more than for any other diagnosis.(3)
Case in point: The use of acupuncture is growing. Its use in the United States tripled between 1997 and 2007. In addition, the research base for acupuncture is rapidly expanding. From 1991 to 2009, nearly 4000 acupuncture research studies were published, with studies on pain accounting for 41% of the acupuncture literature.(4)
But acupuncture is not without controversy. This is due to a lack of a universally accepted biologic mechanism, theories of use and efficacy based in an alternative medical system (traditional Chinese medicine [TCM]), and conflicting views of the evidence.
This article will help make sense of this growing body of knowledge by summarizing the latest evidence and addressing seven common questions about acupuncture for pain conditions. Applying this information will give you the confidence to counsel patients appropriately and decide if acupuncture fits within their pain management plan.
1. What is acupuncture and how does it work?
Acupuncture, which has a 2000-year history of use, involves inserting needles at various points throughout the body to promote healing and improve function. Although acupuncture represents one piece of TCM (which is a holistic system that also includes herbal medicine, nutrition, meditation, and movement), it is often offered as an independent therapy.
Acupuncture point locations are determined either by using an underlying theoretical framework, such as TCM, or by using anatomic structures, such as muscular trigger points. Providers today often employ a hybrid approach when delivering acupuncture treatment. That is, practitioners may choose point locations based on TCM, but they may combine the practice with local treatments that are based on current knowledge of anatomy. For example, a patient presenting with low back pain may be treated utilizing traditional points located near the ankle and knee, and also by needling active trigger points in the quadratus lumborum muscle.
The mechanism of action. One of the reasons for the continuing controversy surrounding acupuncture is the lack of a clear understanding of its underlying mechanism of action. For centuries the “how” of acupuncture has been explained in poetic terms such as yin, yang, and qi. Only in the past half-century have we begun investigating the potential biologic mechanisms responsible for the physiologic effects seen with acupuncture treatment.
While research has uncovered several interesting theories, how these mechanisms interact to produce therapeutic effects is still unclear. However, looking at various components of the nervous system helps to provide some insight.
Consider the nervous system. One way to conceptualize the mechanisms of acupuncture is to consider the various levels of the nervous system and how each level is affected. In the central nervous system, needling an acupuncture point stimulates the natural endorphin system, altering the pain sensation.5 This effect is reversible with naloxone in animal models, indicating that blocking the endorphin system interferes with the analgesic benefits of acupuncture.(5)
Serotonergic systems are also involved centrally. Functional magnetic resonance imaging studies have shown that needling specific acupuncture points modulates areas of the brain.
In the spinal cord, the gate control theory is believed to play a role. (The gate control theory puts forth that nonpainful input closes the “gates” to painful input, which prevents pain sensations from traveling to the central nervous system.) Modulation of sensory input occurs at the level of the dorsal horn of the spinal cord during an acupuncture treatment, which can affect the physiologic pain response.(6) Opioid receptors are also affected at the spinal cord level.(7)
Acupuncture use in the United States tripled between 1997 and 2007.
Lastly, multiple chemicals released peripherally, including interleukins, substance P, and adenosine, appear to contribute to acupuncture’s analgesia.6 We know this because a local anesthetic injected around a peripheral nerve at an acupoint blocks the analgesic effect of acupuncture.(8) Taken together, acupuncture treatment produces physiologic changes in the brain, spinal cord, and at the periphery, making it a truly unique therapeutic modality.
2. Is acupuncture an effective treatment for pain?
Yes, but before we look at the individual studies, it is important to mention some of the shortcomings of the research to date. First, acupuncture trials lack a standard sham control intervention. Some sham treatments involve skin penetration, while others do not. This has led to controversy regarding whether the sham interventions themselves are physiologically active, thus lessening the magnitude of effect for acupuncture. This is a point of contention in the acupuncture literature and a factor to consider when deciding if results have clinical significance.
In addition, the acupuncturist providing treatment in a trial is typically unblinded. This is also true of trials measuring other physical modalities, but it contributes to the debate surrounding the magnitude of placebo response in acupuncture studies.
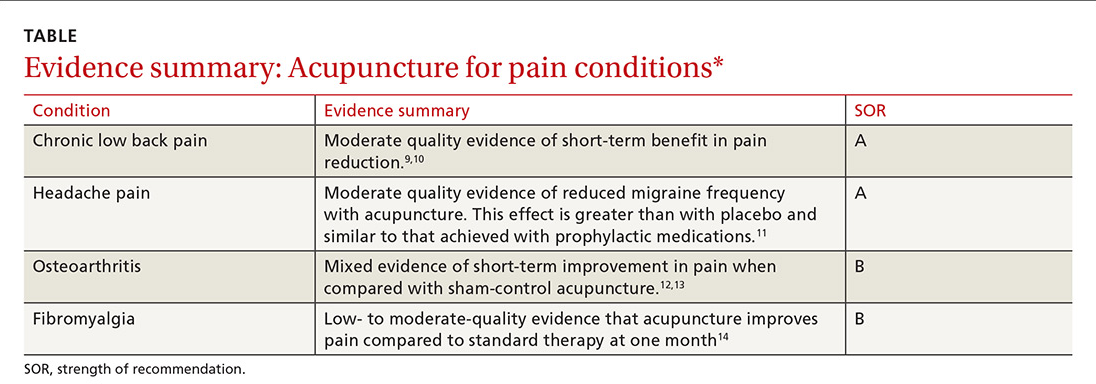
Finally, many randomized trials involving acupuncture have had low methodologic quality. Fortunately, there are now several high-quality systematic reviews that have attempted to filter out the lower-quality research and provide a better representation of the evidence (TABLE). A discussion of them follows.
Author(s): Russell Lemmon, DO
Author and Disclosure Information: Is acupuncture an effective treatment for pain? Are there any adverse effects? Learn the answers to these and other questions in this review.
PRACTICE RECOMMENDATIONS
Recommend acupuncture as a prophylactic treatment for migraine headaches. A
Recommend acupuncture as a treatment option for chronic low back pain. A
Consider using acupuncture as an adjunctive treatment in the management of fibromyalgia symptoms. B
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
An estimated 39.4 million US adults suffer from persistent pain,(1) and the National Institutes of Health indicate that pain affects more Americans than diabetes, heart disease, and cancer combined.(2)
As physicians, we know that conventional options to manage chronic pain leave much to be desired and that more evidence-based treatment options are sorely needed. Patients know this, too, and turn to complementary therapies for pain more than for any other diagnosis.(3)
Case in point: The use of acupuncture is growing. Its use in the United States tripled between 1997 and 2007. In addition, the research base for acupuncture is rapidly expanding. From 1991 to 2009, nearly 4000 acupuncture research studies were published, with studies on pain accounting for 41% of the acupuncture literature.(4)
But acupuncture is not without controversy. This is due to a lack of a universally accepted biologic mechanism, theories of use and efficacy based in an alternative medical system (traditional Chinese medicine [TCM]), and conflicting views of the evidence.
This article will help make sense of this growing body of knowledge by summarizing the latest evidence and addressing seven common questions about acupuncture for pain conditions. Applying this information will give you the confidence to counsel patients appropriately and decide if acupuncture fits within their pain management plan.
1. What is acupuncture and how does it work?
Acupuncture, which has a 2000-year history of use, involves inserting needles at various points throughout the body to promote healing and improve function. Although acupuncture represents one piece of TCM (which is a holistic system that also includes herbal medicine, nutrition, meditation, and movement), it is often offered as an independent therapy.
Acupuncture point locations are determined either by using an underlying theoretical framework, such as TCM, or by using anatomic structures, such as muscular trigger points. Providers today often employ a hybrid approach when delivering acupuncture treatment. That is, practitioners may choose point locations based on TCM, but they may combine the practice with local treatments that are based on current knowledge of anatomy. For example, a patient presenting with low back pain may be treated utilizing traditional points located near the ankle and knee, and also by needling active trigger points in the quadratus lumborum muscle.
The mechanism of action. One of the reasons for the continuing controversy surrounding acupuncture is the lack of a clear understanding of its underlying mechanism of action. For centuries the “how” of acupuncture has been explained in poetic terms such as yin, yang, and qi. Only in the past half-century have we begun investigating the potential biologic mechanisms responsible for the physiologic effects seen with acupuncture treatment.
While research has uncovered several interesting theories, how these mechanisms interact to produce therapeutic effects is still unclear. However, looking at various components of the nervous system helps to provide some insight.
Consider the nervous system. One way to conceptualize the mechanisms of acupuncture is to consider the various levels of the nervous system and how each level is affected. In the central nervous system, needling an acupuncture point stimulates the natural endorphin system, altering the pain sensation.5 This effect is reversible with naloxone in animal models, indicating that blocking the endorphin system interferes with the analgesic benefits of acupuncture.(5)
Serotonergic systems are also involved centrally. Functional magnetic resonance imaging studies have shown that needling specific acupuncture points modulates areas of the brain.
In the spinal cord, the gate control theory is believed to play a role. (The gate control theory puts forth that nonpainful input closes the “gates” to painful input, which prevents pain sensations from traveling to the central nervous system.) Modulation of sensory input occurs at the level of the dorsal horn of the spinal cord during an acupuncture treatment, which can affect the physiologic pain response.(6) Opioid receptors are also affected at the spinal cord level.(7)
Acupuncture use in the United States tripled between 1997 and 2007.
Lastly, multiple chemicals released peripherally, including interleukins, substance P, and adenosine, appear to contribute to acupuncture’s analgesia.6 We know this because a local anesthetic injected around a peripheral nerve at an acupoint blocks the analgesic effect of acupuncture.(8) Taken together, acupuncture treatment produces physiologic changes in the brain, spinal cord, and at the periphery, making it a truly unique therapeutic modality.
2. Is acupuncture an effective treatment for pain?
Yes, but before we look at the individual studies, it is important to mention some of the shortcomings of the research to date. First, acupuncture trials lack a standard sham control intervention. Some sham treatments involve skin penetration, while others do not. This has led to controversy regarding whether the sham interventions themselves are physiologically active, thus lessening the magnitude of effect for acupuncture. This is a point of contention in the acupuncture literature and a factor to consider when deciding if results have clinical significance.
In addition, the acupuncturist providing treatment in a trial is typically unblinded. This is also true of trials measuring other physical modalities, but it contributes to the debate surrounding the magnitude of placebo response in acupuncture studies.
Finally, many randomized trials involving acupuncture have had low methodologic quality. Fortunately, there are now several high-quality systematic reviews that have attempted to filter out the lower-quality research and provide a better representation of the evidence (TABLE). A discussion of them follows.
General chronic pain. A 2012 meta-analysis15 evaluated the effectiveness of acupuncture for the treatment of chronic pain with one of 4 etiologies: nonspecific back or neck pain, chronic headache, osteoarthritis, and shoulder pain. This analysis attempted to control for the high variability of study quality in the acupuncture literature by including only studies of high methodologic character. The final analysis included 29 randomized controlled trials (N=17,922). The authors concluded that acupuncture was superior to both no acupuncture and sham (placebo) acupuncture for all pain conditions in the study. The average effect size was 0.5 standard deviations on a 10-point scale. The authors considered this to be clinically relevant, although the magnitude of benefit was modest.(15)
Low back pain. A 2017 systematic review by Chou et al(9) evaluated 32 trials (N=5931) reviewing acupuncture for the treatment of chronic low back pain. This review found acupuncture was associated with lower pain intensity and improved function in the short term when compared with no treatment. And while acupuncture was associated with lower pain intensity when compared with a sham control, there was no difference in function between the 2 groups. Of note, 3 of the included trials compared acupuncture to standard medications used in the treatment of low back pain and found acupuncture to be superior in terms of both pain reduction and improved function.(9)
Trials that compared acupuncture to another active therapy have found that it often has fewer adverse effects.
The authors of a 2008 systematic review that evaluated 23 trials (N=6359)10 similarly concluded that there is moderate evidence for the use of acupuncture (compared to no treatment) for the treatment of nonspecific low back pain, but did not find evidence that acupuncture was superior to sham controls.(10) The 2017 American College of Physicians clinical practice guidelines support the use of acupuncture for the treatment of chronic low back pain.(16)
In addition to helping with chronic low back pain, acupuncture is also showing promise as a treatment for acute spinal pain. A 2013 systematic review (11 trials, N=1139) showed that acupuncture may be more effective than nonsteroidal anti-inflammatory drugs (NSAIDs) in treating acute low back pain and may cause fewer adverse effects.(17)
Headache pain. Evidence favoring acupuncture in the management of headache has been fairly consistent over the past decade. An updated Cochrane review on the prevention of migraine headaches was published in 2016.(11) Acupuncture was compared with no treatment in 4 trials (n=2199). The authors found moderate quality evidence that acupuncture reduces headache frequency (number needed to treat=4). Acupuncture achieved at least 50% headache reduction in 41% vs 17% in the groups that received no acupuncture. When compared with sham control groups (10 trials, n=1534), acupuncture demonstrated a small but statistically significant improvement in headache frequency. Three trials (n=744) compared acupuncture to medication prophylaxis for migraine headaches and found acupuncture had similar effectiveness with fewer adverse effects.(11)
Osteoarthritis (OA). Most studies have focused on OA of the knee, and, thus far, have generated conflicting results. A Cochrane review in 2010 included 4 trials (n=884) that had a wait list control and 9 trials (n=1835) that compared acupuncture to a sham control.(12) When compared to a wait list control, acupuncture resulted in statistically significant and clinically relevant improvement in pain and function. However, when compared to sham treatment for OA, the review showed statistically significant improvement in pain and function for acupuncture that was unlikely to be clinically relevant.(12)
A more recent meta-analysis in 2016 evaluated 10 trials (N=2007) investigating acupuncture in the treatment of knee OA.13 The authors found acupuncture improved both pain and functional outcome measures when compared with either no treatment or a sham control.
Fibromyalgia. Systematic reviews in 2007 (5 trials, N=316)18 and 2010 (7 trials, N=385)19 showed that acupuncture did provide short-term pain relief in patients with fibromyalgia, but that the effect was not sustained at follow-up. These reviews were limited by a high risk of bias, which was noted in the studies. The authors of both reviews concluded that acupuncture could not be recommended for the treatment of fibromyalgia.
A more recent Cochrane review published in 2013 (9 trials, N=395) offered low- to moderate-level evidence of benefit for acupuncture compared with no treatment at one month follow-up.(14) Of note, there was also evidence of benefit in improved sleep and global well-being, in addition to pain and stiffness measures in this review. The overall magnitude of benefit was small, but clinically significant. Acupuncture also has evidence of benefit in the treatment of conditions commonly seen in conjunction with fibromyalgia, including headaches and low back pain as described earlier.
3. What does a typical acupuncture treatment entail?
In a typical treatment, anywhere from about 5 to 20 needles are inserted into the body. Common areas of needling include the arms and legs, especially below the elbows and knees. Other frequently used areas are the scalp, ears, and structures related to the painful condition.
The needles used are very thin (typically smaller than a 30-gauge needle) and do not have a beveled tip like phlebotomy needles do. Most patients have minimal pain as the needles are inserted. During the treatment, the needles may be left alone or they may be heated or stimulated electrically. An average treatment lasts 30 to 40 minutes; many patients find the sessions relaxing.
4. Are there any adverse effects or complications of treatment?
Acupuncture is generally considered a safe therapy, with most patients experiencing no adverse effects at all. Minor adverse effects can include post-treatment fatigue, minor bruising, or vasovagal reactions from the insertion of the needles. Serious complications, such as pneumothorax, are possible, but are considered rare.(20) A 2004 study estimated the incidence of severe complications to be .05 per 10,000 acupuncture treatments.(21)
Infections are also possible, but most reported cases were due to practitioners reusing needles.(22) The standard of care in the United States is to use only sterilized, single-use needles. With this practice, infections due to acupuncture are thought to be rare.
Of note, trials that compare acupuncture to another active therapy often find that acupuncture has fewer adverse effects. This has been the case when acupuncture was compared to NSAIDs for low back pain and to topiramate for headaches.(17,23)
5. How does acupuncture fit into a patient’s treatment?
The simple answer is that it is often most effectively used as part of a comprehensive management plan for chronic pain.
As our understanding of the complexity of chronic pain deepens, our therapeutic armamentarium for the management of chronic pain needs to broaden. This was summed up well in a 2016 article on the multimodal management of chronic pain when the authors stated, “Many targets need more than one arrow.”(24) Effective management of chronic pain involves addressing psychosocial and lifestyle factors in a patient-centered way and finding a combination of treatments that most effectively leads to improved coping and function.
It’s important to note that like medications and injections, acupuncture is a passive therapy. Although there is evidence for efficacy of improved pain with acupuncture in certain conditions, it should be combined with treatments that actively engage patients, such as exercise, behavioral treatments, development of coping skills, sleep hygiene, and educational strategies.
6. To whom do I refer patients for acupuncture treatment?
In the United States, licensed acupuncturists and physicians most commonly perform acupuncture. There are more than 50 schools that train licensed acupuncturists in the United States, and it usually takes 3 years to meet the requirements.(25)
Licensure varies by state.
7. Is acupuncture covered by insurance?
Patients can expect to pay $75 to $150 for an acupuncture session.
It depends. Insurance coverage of acupuncture is highly variable and based on region and insurance type. Medicare and Medicaid plans pay for acupuncture under certain conditions. There are some private insurance plans that do. If covered, there may be limitations regarding diagnosis, number of visits, or provider. It is best for patients to call their insurance plan directly to inquire about coverage and any limitations. If paying out of pocket, patients can expect to pay $75 to $150 per treatment session.
(Back to top of page)
Go to Richard A Connell, DOM, LAC Homepage
References
1. Kennedy J, Roll JM, Schraudner T, et al. Prevalence of persistent pain in the U.S. adult population: new data from the 2010 National Health Interview Survey. J Pain. 2014;15:979-984.
2. U.S. Department of Health and Human Services. NIH Fact Sheet. Pain management. Available at: https://www.report.nih.gov/nihfactsheets/ViewFactSheet.aspx?csid=57. Accessed February 12, 2018.
3. Barnes PM, Bloom B, Nahin RL. Complementary and alternative medicine use among adults and children: United States, 2007. Natl Health Stat Report. 2008;12:1-23.
4. Nahin RL, Barnes PM, Stussman BJ, et al. Costs of complementary and alternative medicine (CAM) and frequency of visits to CAM practitioners: United States, 2007. Natl Health Stat Report. 2009;18:1-14.
5. Mayer DJ, Price DD, Rafii A. Antagonism of acupuncture analgesia in man by the narcotic antagonist naloxone. Brain Res. 1977;121:368-372.
6. Ammendolia C, Furlan AD, Imamura M, et al. Evidence-informed management of chronic low back pain with needle acupuncture. Spine J. 2008;8:160-172.
7. Zhang R, Lao L, Ren K, et al. Mechanisms of acupuncture-electroacupuncture on persistent pain. Anesthesiology. 2014;120:482-503.
8. Han JS. Acupuncture analgesia: areas of consensus and controversy. Pain. 2011;152(3 Suppl):S41-S48.
9. Chou R, Deyo R, Friedly J, et al. Nonpharmacologic therapies for low back pain: a systematic review for an American College of Physicians clinical practice guideline. Ann Intern Med. 2017;166:493-505.
10. Yuan J, Purepong N, Kerr DP, et al. Effectiveness of acupuncture for low back pain: a systematic review. Spine (Phila Pa 1976). 2008;33:E887-E900.
11. Linde K, Allais G, Brinkhaus B, et al. Acupuncture for the prevention of episodic migraine. Cochrane Database Syst Rev. 2016;6:CD001218.
12. Manheimer E, Cheng K, Linde K, et al. Acupuncture for peripheral joint osteoarthritis. Cochrane Database Syst Rev. 2010;1:CD001977.
13. Lin X, Huang K, Zhu G, et al. The effects of acupuncture on chronic knee pain due to osteoarthritis: a meta-analysis. J Bone Joint Surg Am. 2016;98:1578-1585.
14. Deare JC, Zheng Z, Xue CC, et al. Acupuncture for treating fibromyalgia. Cochrane Database Syst Rev. 2013;5:CD007070.
15. Vickers AJ, Cronin AM, Maschino AC, et al. Acupuncture for chronic pain: individual patient data meta-analysis. Arch Intern Med. 2012;172:1444-1453.
16. Qaseem A, Wilt TJ, McLean RM, et al, for the Clinical Guidelines Committee of the American College of Physicians. Noninvasive treatments for acute, subacute, and chronic low back pain: a clinical practice guideline from the American College of Physicians. Ann Intern Med. 2017;166:514-530.
17. Lee JH, Choi TY, Lee MS, et al. Acupuncture for acute low back pain: a systematic review. Clin J Pain. 2013;29:172-185.
18. Mayhew E, Ernst E. Acupuncture for fibromyalgia—a systematic review of randomized clinical trials. Rheumatology (Oxford). 2007;46:801-804.
19. Langhorst J, Klose P, Musial F, et al. Efficacy of acupuncture in fibromyalgia syndrome—a systematic review with a meta-analysis of controlled clinical trials. Rheumatology (Oxford). 2010;49:778-788.
20. Lao L, Hamilton GR, Fu J, et al. Is acupuncture safe? A systematic review of case reports. Altern Ther Health Med. 2003;9:72-83.
21. White A. A cumulative review of the range and incidence of significant adverse events associated with acupuncture. Acupunct Med. 2004;22:122-133.
22. Xu S, Wang L, Cooper E, et al. Adverse events of acupuncture: a systematic review of case reports. Evid Based Complement Alternat Med. 2013:581203.
23. Linde K, Allais G, Brinkhaus B, et al. Acupuncture for migraine prophylaxis. Cochrane Database Syst Rev. 2009;1:CD001218.
24. Dale R, Stacey B. Multimodal treatment of chronic pain. Med Clin North Am. 2016;100:55-64.
25. National Certification Commission for Acupuncture and Oriental Medicine. Available at: www.nccaom.org. Accessed March 20, 2018.
(Back to top of page)
Low back pain. A 2017 systematic review by Chou et al(9) evaluated 32 trials (N=5931) reviewing acupuncture for the treatment of chronic low back pain. This review found acupuncture was associated with lower pain intensity and improved function in the short term when compared with no treatment. And while acupuncture was associated with lower pain intensity when compared with a sham control, there was no difference in function between the 2 groups. Of note, 3 of the included trials compared acupuncture to standard medications used in the treatment of low back pain and found acupuncture to be superior in terms of both pain reduction and improved function.(9)
Trials that compared acupuncture to another active therapy have found that it often has fewer adverse effects.
The authors of a 2008 systematic review that evaluated 23 trials (N=6359)10 similarly concluded that there is moderate evidence for the use of acupuncture (compared to no treatment) for the treatment of nonspecific low back pain, but did not find evidence that acupuncture was superior to sham controls.(10) The 2017 American College of Physicians clinical practice guidelines support the use of acupuncture for the treatment of chronic low back pain.(16)
In addition to helping with chronic low back pain, acupuncture is also showing promise as a treatment for acute spinal pain. A 2013 systematic review (11 trials, N=1139) showed that acupuncture may be more effective than nonsteroidal anti-inflammatory drugs (NSAIDs) in treating acute low back pain and may cause fewer adverse effects.(17)
Headache pain. Evidence favoring acupuncture in the management of headache has been fairly consistent over the past decade. An updated Cochrane review on the prevention of migraine headaches was published in 2016.(11) Acupuncture was compared with no treatment in 4 trials (n=2199). The authors found moderate quality evidence that acupuncture reduces headache frequency (number needed to treat=4). Acupuncture achieved at least 50% headache reduction in 41% vs 17% in the groups that received no acupuncture. When compared with sham control groups (10 trials, n=1534), acupuncture demonstrated a small but statistically significant improvement in headache frequency. Three trials (n=744) compared acupuncture to medication prophylaxis for migraine headaches and found acupuncture had similar effectiveness with fewer adverse effects.(11)
Osteoarthritis (OA). Most studies have focused on OA of the knee, and, thus far, have generated conflicting results. A Cochrane review in 2010 included 4 trials (n=884) that had a wait list control and 9 trials (n=1835) that compared acupuncture to a sham control.(12) When compared to a wait list control, acupuncture resulted in statistically significant and clinically relevant improvement in pain and function. However, when compared to sham treatment for OA, the review showed statistically significant improvement in pain and function for acupuncture that was unlikely to be clinically relevant.(12)
A more recent meta-analysis in 2016 evaluated 10 trials (N=2007) investigating acupuncture in the treatment of knee OA.13 The authors found acupuncture improved both pain and functional outcome measures when compared with either no treatment or a sham control.
Fibromyalgia. Systematic reviews in 2007 (5 trials, N=316)18 and 2010 (7 trials, N=385)19 showed that acupuncture did provide short-term pain relief in patients with fibromyalgia, but that the effect was not sustained at follow-up. These reviews were limited by a high risk of bias, which was noted in the studies. The authors of both reviews concluded that acupuncture could not be recommended for the treatment of fibromyalgia.
A more recent Cochrane review published in 2013 (9 trials, N=395) offered low- to moderate-level evidence of benefit for acupuncture compared with no treatment at one month follow-up.(14) Of note, there was also evidence of benefit in improved sleep and global well-being, in addition to pain and stiffness measures in this review. The overall magnitude of benefit was small, but clinically significant. Acupuncture also has evidence of benefit in the treatment of conditions commonly seen in conjunction with fibromyalgia, including headaches and low back pain as described earlier.
3. What does a typical acupuncture treatment entail?
In a typical treatment, anywhere from about 5 to 20 needles are inserted into the body. Common areas of needling include the arms and legs, especially below the elbows and knees. Other frequently used areas are the scalp, ears, and structures related to the painful condition.
The needles used are very thin (typically smaller than a 30-gauge needle) and do not have a beveled tip like phlebotomy needles do. Most patients have minimal pain as the needles are inserted. During the treatment, the needles may be left alone or they may be heated or stimulated electrically. An average treatment lasts 30 to 40 minutes; many patients find the sessions relaxing.
4. Are there any adverse effects or complications of treatment?
Acupuncture is generally considered a safe therapy, with most patients experiencing no adverse effects at all. Minor adverse effects can include post-treatment fatigue, minor bruising, or vasovagal reactions from the insertion of the needles. Serious complications, such as pneumothorax, are possible, but are considered rare.(20) A 2004 study estimated the incidence of severe complications to be .05 per 10,000 acupuncture treatments.(21)
Infections are also possible, but most reported cases were due to practitioners reusing needles.(22) The standard of care in the United States is to use only sterilized, single-use needles. With this practice, infections due to acupuncture are thought to be rare.
Of note, trials that compare acupuncture to another active therapy often find that acupuncture has fewer adverse effects. This has been the case when acupuncture was compared to NSAIDs for low back pain and to topiramate for headaches.(17,23)
5. How does acupuncture fit into a patient’s treatment?
The simple answer is that it is often most effectively used as part of a comprehensive management plan for chronic pain.
As our understanding of the complexity of chronic pain deepens, our therapeutic armamentarium for the management of chronic pain needs to broaden. This was summed up well in a 2016 article on the multimodal management of chronic pain when the authors stated, “Many targets need more than one arrow.”(24) Effective management of chronic pain involves addressing psychosocial and lifestyle factors in a patient-centered way and finding a combination of treatments that most effectively leads to improved coping and function.
It’s important to note that like medications and injections, acupuncture is a passive therapy. Although there is evidence for efficacy of improved pain with acupuncture in certain conditions, it should be combined with treatments that actively engage patients, such as exercise, behavioral treatments, development of coping skills, sleep hygiene, and educational strategies.
6. To whom do I refer patients for acupuncture treatment?
In the United States, licensed acupuncturists and physicians most commonly perform acupuncture. There are more than 50 schools that train licensed acupuncturists in the United States, and it usually takes 3 years to meet the requirements.(25)
Licensure varies by state.
7. Is acupuncture covered by insurance?
Patients can expect to pay $75 to $150 for an acupuncture session.
It depends. Insurance coverage of acupuncture is highly variable and based on region and insurance type. Medicare and Medicaid plans pay for acupuncture under certain conditions. There are some private insurance plans that do. If covered, there may be limitations regarding diagnosis, number of visits, or provider. It is best for patients to call their insurance plan directly to inquire about coverage and any limitations. If paying out of pocket, patients can expect to pay $75 to $150 per treatment session.
(Back to top of page)
Go to Richard A Connell, DOM, LAC Homepage
References
1. Kennedy J, Roll JM, Schraudner T, et al. Prevalence of persistent pain in the U.S. adult population: new data from the 2010 National Health Interview Survey. J Pain. 2014;15:979-984.
2. U.S. Department of Health and Human Services. NIH Fact Sheet. Pain management. Available at: https://www.report.nih.gov/nihfactsheets/ViewFactSheet.aspx?csid=57. Accessed February 12, 2018.
3. Barnes PM, Bloom B, Nahin RL. Complementary and alternative medicine use among adults and children: United States, 2007. Natl Health Stat Report. 2008;12:1-23.
4. Nahin RL, Barnes PM, Stussman BJ, et al. Costs of complementary and alternative medicine (CAM) and frequency of visits to CAM practitioners: United States, 2007. Natl Health Stat Report. 2009;18:1-14.
5. Mayer DJ, Price DD, Rafii A. Antagonism of acupuncture analgesia in man by the narcotic antagonist naloxone. Brain Res. 1977;121:368-372.
6. Ammendolia C, Furlan AD, Imamura M, et al. Evidence-informed management of chronic low back pain with needle acupuncture. Spine J. 2008;8:160-172.
7. Zhang R, Lao L, Ren K, et al. Mechanisms of acupuncture-electroacupuncture on persistent pain. Anesthesiology. 2014;120:482-503.
8. Han JS. Acupuncture analgesia: areas of consensus and controversy. Pain. 2011;152(3 Suppl):S41-S48.
9. Chou R, Deyo R, Friedly J, et al. Nonpharmacologic therapies for low back pain: a systematic review for an American College of Physicians clinical practice guideline. Ann Intern Med. 2017;166:493-505.
10. Yuan J, Purepong N, Kerr DP, et al. Effectiveness of acupuncture for low back pain: a systematic review. Spine (Phila Pa 1976). 2008;33:E887-E900.
11. Linde K, Allais G, Brinkhaus B, et al. Acupuncture for the prevention of episodic migraine. Cochrane Database Syst Rev. 2016;6:CD001218.
12. Manheimer E, Cheng K, Linde K, et al. Acupuncture for peripheral joint osteoarthritis. Cochrane Database Syst Rev. 2010;1:CD001977.
13. Lin X, Huang K, Zhu G, et al. The effects of acupuncture on chronic knee pain due to osteoarthritis: a meta-analysis. J Bone Joint Surg Am. 2016;98:1578-1585.
14. Deare JC, Zheng Z, Xue CC, et al. Acupuncture for treating fibromyalgia. Cochrane Database Syst Rev. 2013;5:CD007070.
15. Vickers AJ, Cronin AM, Maschino AC, et al. Acupuncture for chronic pain: individual patient data meta-analysis. Arch Intern Med. 2012;172:1444-1453.
16. Qaseem A, Wilt TJ, McLean RM, et al, for the Clinical Guidelines Committee of the American College of Physicians. Noninvasive treatments for acute, subacute, and chronic low back pain: a clinical practice guideline from the American College of Physicians. Ann Intern Med. 2017;166:514-530.
17. Lee JH, Choi TY, Lee MS, et al. Acupuncture for acute low back pain: a systematic review. Clin J Pain. 2013;29:172-185.
18. Mayhew E, Ernst E. Acupuncture for fibromyalgia—a systematic review of randomized clinical trials. Rheumatology (Oxford). 2007;46:801-804.
19. Langhorst J, Klose P, Musial F, et al. Efficacy of acupuncture in fibromyalgia syndrome—a systematic review with a meta-analysis of controlled clinical trials. Rheumatology (Oxford). 2010;49:778-788.
20. Lao L, Hamilton GR, Fu J, et al. Is acupuncture safe? A systematic review of case reports. Altern Ther Health Med. 2003;9:72-83.
21. White A. A cumulative review of the range and incidence of significant adverse events associated with acupuncture. Acupunct Med. 2004;22:122-133.
22. Xu S, Wang L, Cooper E, et al. Adverse events of acupuncture: a systematic review of case reports. Evid Based Complement Alternat Med. 2013:581203.
23. Linde K, Allais G, Brinkhaus B, et al. Acupuncture for migraine prophylaxis. Cochrane Database Syst Rev. 2009;1:CD001218.
24. Dale R, Stacey B. Multimodal treatment of chronic pain. Med Clin North Am. 2016;100:55-64.
25. National Certification Commission for Acupuncture and Oriental Medicine. Available at: www.nccaom.org. Accessed March 20, 2018.
(Back to top of page)
We Welcome Referrals
Physicians and other healthcare providers are encouraged to refer patients to our pain clinic for primary treatment as well as secondary or post surgery rehabilitation.
If you require information specific to Richard A Connell, DOM, LAC, his acupuncture clinic in Galena or about the therapies we provide, you are welcome to click here to check out our front page page or call us at (815) 238 3803 to speak with our office directly.
© 2001-2025 CONSCIOUS HEALTH, LLC - DBA RICHARD A CONNELL, DOM, LICENSED ACUPUNCTURIST - 11400 US-20 W, #4 Galena, Illinois 61036 PH: 815 238 3803